In this article:
- How does food affect my hemodialysis?
- What do I need to know about fluids?
- What do I need to know about potassium?
- What do I need to know about phosphorus?
- What do I need to know about protein?
- What do I need to know about sodium?
- What do I need to know about calories?
- Should I take vitamins and minerals?
- Resources
- Acknowledgments
When you start hemodialysis, you must make many changes in your life. Watching the foods you eat will make you healthier. This article will help you choose the right foods. Print this page and use it with a dietitian to help you learn how to eat right to feel right on hemodialysis. Read one section at a time. Then go through the exercise with your dietitian. Once you have completed every exercise, keep a copy of this article to remind yourself of foods you can eat and foods you need to avoid.
My dietitian's name is _____________________________
Phone ___________________
How does food affect my hemodialysis?
Food gives you energy and helps your body repair itself. Food is broken down in your stomach and intestines. Your blood picks up nutrients from the digested food and carries them to all your body cells. These cells take nutrients from your blood and put waste products back into the bloodstream. When your kidneys were healthy, they worked around the clock to remove wastes from your blood. The wastes left your body when you urinated. Other wastes are removed in bowel movements.
Now your kidneys have stopped working. Hemodialysis removes wastes from your blood. But between sessions, wastes can build up in your blood and make you sick. You can reduce the amount of wastes by watching what you eat and drink. A good meal plan can improve your dialysis and your health.
Your clinic has a dietitian to help you plan meals. A dietitian specializes in food and nutrition. A dietitian with special training in care for kidney health is called a renal dietitian. Talk to a dietitian to learn how to eat right on hemodialysis.
[Top]What do I need to know about fluids?
You already know you need to watch how much you drink. Any food that is liquid at room temperature also contains water. These foods include soup, Jell-O, and ice cream. Many fruits and vegetables contain lots of water, too. They include melons, grapes, apples, oranges, tomatoes, lettuce, and celery. All these foods add to your fluid intake.
Fluid can build up between dialysis sessions, causing swelling and weight gain. The extra fluid affects your blood pressure and can make your heart work harder. You could get serious heart trouble from overloading your system with fluid.
Control Your ThirstYou can keep your fluids down by drinking from smaller cups or glasses. Freeze juice in an ice cube tray and eat it like a popsicle. (Remember to count the popsicle in your fluid allowance!) The dietitian will be able to give you other tips for managing your thirst. |
Your dry weight is your weight after a dialysis session when all of the extra fluid in your body has been removed. If you let too much fluid build up between sessions, it is harder to get down to your proper dry weight. Your dry weight may change over a period of 3 to 6 weeks. Talk to your doctor regularly about what your dry weight should be.
My dry weight should be _____________.
| Many foods contain water: |
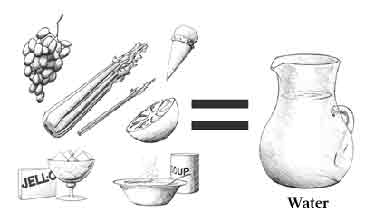 |
Talk to a DietitianEven though you are on hemodialysis, your kidneys may still be able to remove some fluid. Or your kidneys may not remove any fluid at all. That is why every patient has a different daily allowance for fluid. Talk to your dietitian about how much fluid you can have each day. I can have _____ ounces of fluid each day. Plan 1 day of fluid servings: I can have _____ ounce(s) of ______________ with breakfast. I can have _____ ounce(s) of ______________ in the morning. I can have _____ ounce(s) of ______________ with lunch. I can have _____ ounce(s) of ______________ in the afternoon. I can have _____ ounce(s) of ______________ with supper. I can have _____ ounce(s) of ______________ in the evening. TOTAL _______ ounces (should equal the allowance written above) |
 |
| Be careful to keep track of your fluids and other foods. |
[Top]
What do I need to know about potassium?
Potassium is a mineral found in many foods, especially milk, fruits, and vegetables. It affects how steadily your heart beats. Healthy kidneys keep the right amount of potassium in the blood to keep the heart beating at a steady pace. Potassium levels can rise between dialysis sessions and affect your heartbeat. Eating too much potassium can be very dangerous to your heart. It may even cause death.
You can remove some potassium from potatoes by soaking them in water.
To control potassium levels in your blood, avoid foods like avocados, bananas, kiwis, and dried fruit, which are very high in potassium. Also, eat smaller portions of other high-potassium foods. For example, eat half a pear instead of a whole pear. Eat only very small portions of oranges and melons.
Dialyzing Potatoes and Other Vegetables
You can remove some of the potassium from potatoes and other vegetables by peeling them, then soaking them in a large amount of water for several hours. Drain and rinse before cooking. Your dietitian will give you more specific information about the potassium content of foods.
|
[Top]
What do I need to know about phosphorus?
Phosphorus is a mineral found in many foods. If you have too much phosphorus in your blood, it pulls calcium from your bones. Losing calcium will make your bones weak and likely to break. Also, too much phosphorus may make your skin itch. Foods like milk and cheese, dried beans, peas, colas, nuts, and peanut butter are high in phosphorus. Usually, people on dialysis are limited to 1/2 cup of milk per day. The renal dietitian will give you more specific information regarding phosphorus.
You probably will need to take a phosphate binder like Renagel, PhosLo, Tums, or calcium carbonate to control the phosphorus in your blood between dialysis sessions. These medications act like sponges to soak up, or bind, phosphorus while it is in the stomach. Because it is bound, the phosphorus does not get into the blood. Instead, it is passed out of the body in the stool.
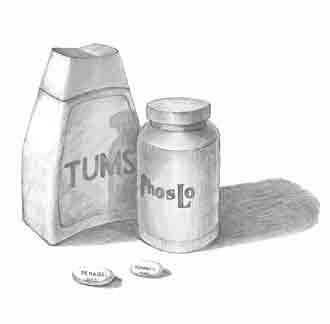
Taking a phosphate binder helps control phosphorus in your blood.
[Top]What do I need to know about protein?
Before you were on dialysis, your doctor may have told you to follow a low-protein diet. Being on dialysis changes this. Most people on dialysis are encouraged to eat as much high-quality protein as they can. The better nourished you are, the healthier you will be. You will also have greater resistance to infection and recover from surgery more quickly.
Protein helps you keep muscle and repair tissue. In your body, protein breaks down into a waste product called urea. If urea builds up in your blood, you can become very sick. Some sources of protein produce less waste than others. These are called high-quality proteins. High-quality proteins come from meat, fish, poultry, and eggs (especially egg whites). Getting most of your protein from these sources can reduce the amount of urea in your blood.
 |
| Poultry and fish, like broiled flounder, are a good source of high-quality protein. |
Talk to a DietitianMeat, fish, and chicken are good sources of protein. Talk to a dietitian about the meats you eat. I will eat ______ servings of meat each day. A regular serving size is 3 ounces. This is about the size of the palm of your hand or a deck of cards. Try to choose lean (low-fat) meats that are also low in phosphorus. If you are a vegetarian, ask about other ways to get your protein. Low-fat milk is a good source of protein. But milk is high in phosphorus and potassium. And milk adds to your fluid intake. Talk to a dietitian to see if milk fits into your food plan. I (will) (will not) drink milk. I will drink ______ cup(s) of milk a day. |
[Top]
What do I need to know about sodium?
Sodium is found in salt and other foods. Most canned foods and frozen dinners contain large amounts of sodium. Too much sodium makes you thirsty. But if you drink more fluid, your heart has to work harder to pump the fluid through your body. Over time, this can cause high blood pressure and congestive heart failure.
Try to eat fresh foods that are naturally low in sodium. Look for products labeled low sodium.
Do not use salt substitutes because they contain potassium. Talk to a dietitian about spices you can use to flavor your food. The dietitian can help you find spice blends without sodium or potassium.
 |
| Find new ways to spice up your food. |
Talk to a DietitianTalk to a dietitian about spices and other healthy foods you can use to flavor your diet. List them on the lines below. Spice: _____________________________ Spice: _____________________________ Spice: _____________________________ Food: _____________________________ Food: _____________________________ |
[Top]
What do I need to know about calories?
Calories provide energy for your body. If your doctor recommends it, you may need to cut down on the calories you eat. A dietitian can help you plan ways to cut calories in the best possible way.
But some people on dialysis need to gain weight. You may need to find ways to add calories to your diet. Vegetable oils�like olive oil, canola oil, and safflower oil�are good sources of calories. Use them generously on breads, rice, and noodles.
Butter and margarines are rich in calories. But these fatty foods can also clog your arteries. Use them less often. Soft margarine that comes in tubs is better than stick margarine. Vegetable oils are the healthiest way to add fat to your diet if you need to gain weight.
Hard candy, sugar, honey, jam, and jelly provide calories and energy without clogging arteries or adding other things that your body does not need. If you have diabetes, be very careful about eating sweets. A dietitian's guidance is very important for people with diabetes.
 |
| If you need to get extra calories, vegetable oils like these are a good choice. |
[Top]
Should I take vitamins and minerals?
Vitamins and minerals may be missing from your diet because you have to avoid so many foods. Your doctor may prescribe a vitamin and mineral supplement like Nephrocaps.
Warning: Do not take vitamins that you can buy off the store shelf. They may contain vitamins or minerals that are harmful to you. Take only the vitamins your doctor prescribes. [Top]Resources
Books
- Bowes and Church's Food Values of Portions Commonly Used.
Jean A. T. Pennington. J.P. Lippincott Co.
ISBN: 0-397-55435-4. - The Complete Book of Food Counts.
Corinne T. Netzer. Dell Publishing Co.
ISBN: 0-440-22110-2.
Brochures
- Nutrition and Hemodialysis.
National Kidney Foundation
30 East 33rd Street
New York, NY 10016
Phone: 1�800�622�9010 or 212�889�2210 - How to Increase Calories in Your Renal Diet.
National Kidney Foundation
30 East 33rd Street
New York, NY 10016
Phone: 1�800�622�9010 or 212�889�2210
Charts and Posters
- The American Association of Kidney Patients provides an online sodium-potassium-phosphorus counter at aakp.org/AAKP/nakphos.htm.
- Picture Renal Diet. (Poster)
Available from University Hospital, Food and Nutrition Services
619 South 19th Street
Birmingham, AL 35233
Phone: 205�934�8055
Cookbooks
These cookbooks provide recipes for people on dialysis:
- The Renal Gourmet.
Mardy Peters
ISBN: 0-9641730-0-X - Southwest Cookbook for People on Dialysis
Developed by the El Paso Chapter Council on Renal Nutrition and the National Kidney Foundation of Texas, Inc.
Published by a grant from Amgen Inc. Available from:
National Kidney Foundation of Texas
13500 Midway Road, Suite 101
Dallas, TX 75244
Phone: 972�934�8057 - Creative Cooking for Renal Diets
By Cleveland Clinic Found
ISBN: 0941511006 - Creative Cooking for Renal Diabetic Diets
Cleveland Clinic Found
ISBN: 0941511014
Acknowledgments
The individuals listed here provided editorial guidance or facilitated field testing for this article.
- Lawrence Y. Agodoa, M.D.
- Kim Bayer, M.A., R.D., L.D.
- Josephine P. Briggs, M.D.
- Shirley Cox, R.D., L.D.
- Sana Dicey, R.D.
- Laura Byham Gray, M.S., R.D., C.N.S.D.
- Linda Hager, M.S., R.D.
- Melissa Hildebrand, R.D., L.D.
- Lisa Hill, R.D., C.D.E.
- Jean King, R.D., C.D.E.
- Wanda Knopik
- Susan Lindsey-Goldman, R.D.
- Betty Murray, R.N.
- Jean Pennington, Ph.D., R.D.
- Gail Radosevich, R.D., L.D.
- Susan Schommer, R.D., L.D.
- Charlotte Stall, M.A., R.D.
0
NIH






